Orthopedic Massage: The Missing Link in Surgical Care
The Big Day
10:45am - Admission. I watch her limp to the desk. She sits and lets out a slight sigh, of relief I imagine, reaching into her purse for her insurance card and ID. The lobby is bustling. She seems calm.
11:30am - Surgery Prep. We were asked to stay in the family waiting room while the staff prepares her for surgery: hospital gown, cap and socks, IV in her hand, ID bracelet on her wrist. She gave a smile when she saw us coming in. The pre-operative suite is busy. She rests back in the chair patiently.
12:20pm - Pre-op meeting with the surgeon. He was pleasant, professional and apologetic about the delay. Its one of those days, and the previous patient arrived late. There’s no rush since the operation requires an overnight stay. She thanks him as he heads off. She would see him again soon.
12:50pm - Anesthesiologist. No allergies. No past negative experiences. A solid plan of action, and no further questions.
1:24pm - Showtime. We hug, we kiss and say I Love You’s. Surgery expected to take about 2 hours. Enough time for me to get some food and work done. She’s ready, and I’d be there when she was finished.
2:07pm - The procedure has started.
My beautiful mother in her hospital fashions, prepped for surgery and surrounded by love.
How Did We Get Here?
When she arrived in New York from the Virgin Islands at eighteen, she had big plans and a bigger heart. She fell in love, got hired by a great company, and would quickly join the rat race that is the NYC hustle. Dressed to the nines and on the grind, I called her a “corporate athlete”. She spent her working hours at a desk, but her "arena" really was the commute: an hour and a half in each direction, five days a week.
For most, an athletic career is measured in medals, trophies or championship rings. For my mother, it’s measured in city blocks, subway transfers, and millions of steps accumulated through the sun, rain, sleet and snow in New York City.
It was a rhythmic, religious, and relentless routine:
The walk to the bus stop.
The transition to the train.
The climb up and down those dirty subway stairs.
The swift power walk to the building, through the lobby, up the elevator, and to her desk.
Two times a day. Five times a week.
She pounded the pavement for decades and eventually it took its toll. That hustle, her signature power walk, was wearing down the cartilage in her knee.
Help Is On The Way
I traveled from Florida back home to New York, trading the sunshine for the city winter chill, not just to be her daughter, but to be her therapist. As we waited for the surgeons to take over, I knew I had one more job to do. I reached for her leg and began a pre-operative massage. This wasn't just about comfort; it was about preparing the "soil" before the "seeds" of surgery were planted—calming her nervous system, increasing local circulation, and ensuring her body was in a state of ease before the trauma of the incision.
Pre-operative orthopedic massage
3:46pm - The procedure has ended.
The 4 Stages of Healing: A Biological Construction Site
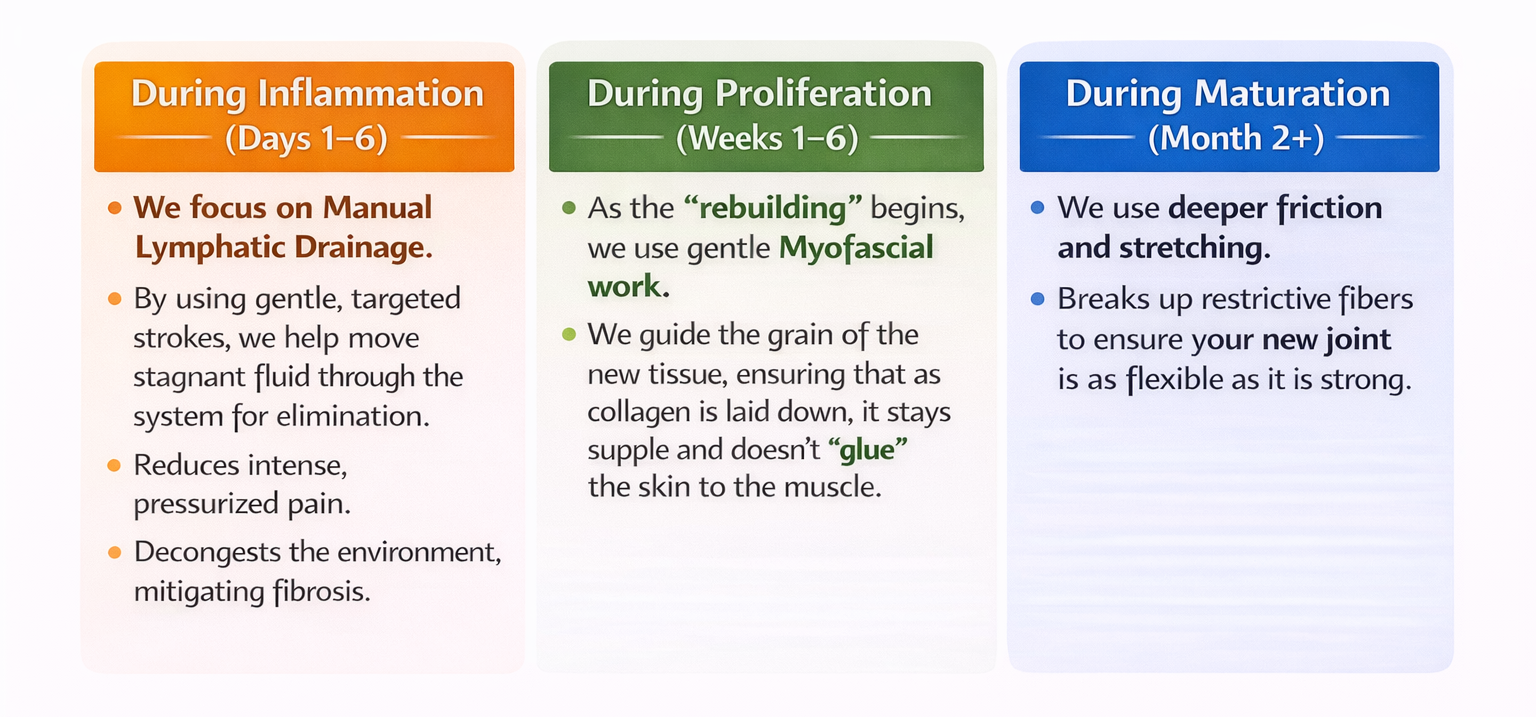
Once the surgeon finishes the mechanical work of the joint replacement, the body’s internal engineering takes over initiating a precise, four-stage reconstruction project. Understanding this timeline is the key to knowing when and how we intervene with massage and manual therapy:
The 4 Stages of Wound Healing
Why Massage is the "Project Manager" of Healing
Without intervention and left to its own devices, the body often over-repairs. The proliferation phase can lead to fibrosis—the formation of excessive, dense fibrous connective tissue. Think of it as internal scarring that is too thick and rigid. Fibrosis creates "adhesions" that act like glue, sticking layers of muscle, nerves, and skin together. This is what causes that bumpy, "leathery" feel under the skin.
By integrating massage into these stages, we act as the project manager for your recovery to manage inflammation, bring nutrient-rich blood to needy tissues, and prevent fibrosis before it takes hold.
Supporting the Whole Athlete: Beyond the Surgical Site
While the surgical knee is the focus, we cannot ignore the rest of the body. During recovery, your biomechanics shift to protect the new joint. This overcompensation often leads to secondary issues that can be just as painful as the surgery itself.
Managing the Overcompensation
The Opposing Leg: This leg becomes the "anchor," bearing the majority of your body weight while the surgical side heals. The hip, quad, and calf of the non-surgical leg often become chronically tight and fatigued. We treat this "supporting leg" to prevent overuse injuries and keep you mobile.
The Lower Back and Hips: Using crutches, a walker, or even just favoring one side changes your gait. This creates a "domino effect" of tension through the pelvis and lumbar spine. We work to release these structures, ensuring your foundation remains balanced.
Managing the Stress of Recovery
Recovery is a high-stress state for the nervous system. The body cannot heal efficiently if it is stuck in a "fight or flight" mode. This is where we integrate Swedish Massage and systemic relaxation techniques. By calming the nervous system, we lower cortisol (the stress hormone that can slow healing) and improve sleep quality—which is when the most significant cellular repair (Maturation) occurs.
Self-Care Tips for a Smooth Recovery
Beyond clinical treatment and professional care, the daily choices you make at home act as the foundation for your new joint's longevity.
The PRICE Protocol: In the acute phase, always return to the gold standard:
Protect: Guard the joint from further trauma or falls.
Rest: Give your body the grace and time it needs to focus energy on repair.
Ice: Use cold therapy to manage swelling, pain, and heat.
Compress: Use compression socks or wraps to manage edema.
Elevate: Keep the knee above the level of your heart to assist lymphatic drainage.
Follow Doctor’s Orders: Stay on top of your medication schedule as prescribed by your surgical team. Managing pain effectively in the early days allows you to participate more fully in the movement required for healing.
Movement is Medicine: Complete stagnation is the enemy of recovery. Follow your physical therapist’s exercise plan religiously. Controlled movement improves circulation, prevents clots, and keeps the joint lubricated.
Anti-Inflammatory Nutrition: Support your body’s rebuilding process by eating foods rich in antioxidants and omega-3s. Leafy greens, berries, fatty fish, and turmeric can help manage systemic inflammation from the inside out.
Prioritize Sleep: This is when the Maturation phase is at its peak. Your body does its heaviest lifting and tissue remodeling while you are in deep sleep.
Manage Stress: Practice deep breathing or meditation. Reducing mental stress keeps your nervous system in the "rest and digest" state necessary for optimal cellular repair.
Mom already on her feet, just a few hours post-operation.
The Recovery Toolkit: Essential Gear for Your Journey
Healing a new joint requires the right environment and the right tools. Based on my clinical experience and my mother's own journey, I have curated a list of essentials from my Amazon Storefront to help you navigate the stages of recovery with more ease and safety.
Mobility & Stability Support: A sturdy Walker and a set of Crutches are your first steps toward independence. To assist with the transition from sitting to standing, a Stand-Up Assist rail provides the necessary leverage.
Elevation & Comfort: A Leg Elevation Pillow is critical for managing the Inflammatory phase. For resting in bed, a Wedge Pillow provides the support needed to sit up without straining your back.
Circulation & Pain Management: Consistent Cold Compresses/Ice Therapy are vital for "quieting" the heat. To support blood flow and prevent stagnant fluid, a quality pair of Compression Socks is a daily must-have.
Hygiene & Safety: A Shower Chair and Waterproof Bandages allow you to maintain your hygiene routine safely. For the days when a full shower is too much, Shower Wipes are a lifesaver.
Independence in the Home: A Grabber Tool prevents you from overextending or bending in ways that could compromise the joint.
Home Recovery & Maintenance: As you move into the Proliferation and Maturation phases, a Handheld Self-Massager, a Foam Roller, and a Vibration Therapy Gun are excellent tools to manage muscle tension between clinical sessions.
A Heartfelt Note of Gratitude
Finally, I want to extend a sincere thank you to the exceptional professionals at NYU Langone Orthopedic. Their expertise and care ensured a successful surgery, providing the foundation upon which this recovery is built. We are deeply grateful for their skill and dedication to helping our loved ones get back to their lives.
Your Journey to Recovery Starts Here
My mother’s journey from the Virgin Islands to the pavement of NYC has been one of incredible strength. Now, her journey is about healing that same strength back into her body.
References & Clinical Resources
Wound Healing Phases: Clinical guidelines provided by the National Center for Biotechnology Information (NCBI) / StatPearls (Stages of Wound Healing).
Manual Therapy for Post-Operative Edema: Research provided by the Journal of Clinical Medicine regarding Manual Lymphatic Drainage (MLD) efficacy.
Arthrofibrosis & Scar Tissue Management: Clinical overview of knee replacement recovery via NYU Langone Health Orthopedics.